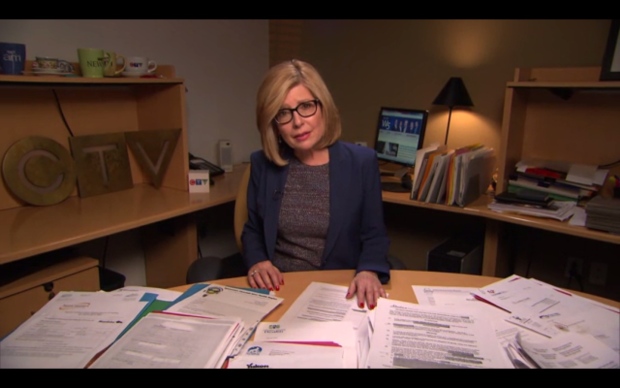
Over the course of a one year investigation, W5 uncovered at least 1,500 cases of staff-to-resident abuse and neglect in nursing homes across Canada in 2013. That number is likely higher due to under-reporting of incidents.
W5 obtained the data by filing access-to-information requests with 42 provincial, territorial and regional health authorities seeking statistical information and incident reports of staff-to-resident abuse for the 2013 calendar year.
Behind the sad statistics are the stories that become sadder when they’re investigated and the details become known.
Three stories are reported in detail in W5’s documentary investigation of abuse and neglect on the part of long-term care home staff.
Hidden cameras capture abuse and questionable care
There is the story of Hellen MacDonald, resident at St. Joseph’s at Fleming in Peterborough, Ont.
Her story gained national prominence when her son, Camille Parent, exposed staff misconduct captured by a hidden camera he installed after nobody at the home could explain his mom’s black eye and bruising.

Troubling images show one staff member wiping his nose on her sheets. In another sequence, two staff members appear to be having a romantic liaison while Helen lies in her bed.

But most troubling is footage of one care worker pushing and roughly handling her and waving a cloth she had just used to clean Helen’s backside in her face.
Four workers were fired by the home, but three regained their jobs after their union fought for their reinstatement.

While St. Joseph declined W5’s interview request, they did say: “We have learned from our past and have implemented change through expanded education, a thorough review of policy and processes, and a fresh approach to care.
There is the story of Eileen Adamson, resident at the Kipnes Centre for Veterans in Edmonton, Alberta who was subjected to rough handling and humiliation at the hands of two employees – shocking behaviour that was captured by a hidden camera installed by her daughter Susan Carter.

The aides are no longer working at the home while the facility and the Alberta government conduct their investigations.

Unanswered questions
And then there is the story of Margaret Warholm, whose family is haunted by the lingering question: How was it that their 74-year-old mother was neglected in the very place they trusted to keep her safe?

Margaret wasn’t well; she had been diagnosed with severe spinal stenosis – the narrowing of the space in our spines that houses the spinal cord and the nervous tissue inside. Margaret was moved into the Santa Maria Senior Citizen’s Home.
As her back condition worsened, she became completely bedridden. Staff members were warned not to move her out of bed for any reason.
But in August 2013, two health care aides somehow dropped her, reportedly while transferring her into a wheelchair.
When Margaret’s daughters asked about the incident, they were told Margaret had suffered a bump on the head.
Margaret told her daughters that the aides had dropped her and that she was scared they would drop her again.
After days of excruciating pain, Margaret was rushed to hospital where doctors learned she didn’t just have a bump on her head. Her spine was fractured in four places.
Hospital nurses also discovered a massive bedsore that covered most of her back. The family was aware Margaret had a bedsore but had been assured by the staff at the nursing home that it was only the size of a quarter.
After a few days in hospital, Margaret Warholm died. Her family believes she lost the will to live after suffering needlessly.
“No one should have to go through that,” said her daughter, Susan Langan, while showing W5 photos of her mother’s massive bedsore.
“We hope we can prevent another family from ever having to look at a picture like this. It was awful.”
In its internal investigation into the incident, Santa Maria Senior Citizens Home cited a “lack of critical thinking” on the part of the staff.
But Margaret Warholm’s family remained upset that the health care aides involved in her care and who had dropped her continue to work at the home.
“When somebody signs up to do that job, they have a moral obligation that they are going to do the best they possibly can to care for that, that person,” said daughter-in-law Leanna MacFarlane. “And if you can’t accept that obligation you shouldn’t be there.”
Santa Maria’s CEO John Kelly assured W5 “the individuals involved have acknowledged they made those mistakes and they’re remorseful.”
“The caregivers were disciplined according to the collective agreement,” Kelly said in an interview with Sandie Rinaldo, while confirming that the staff members continue to be employed at Santa Maria.

Kelly also told W5 said the home has adopted a new resident and family-centered model of care with a focus on improving communications with families.
Access to information
When W5 tried to find out more about incidents across Saskatchewan, and, in particular, inside Santa Maria, by filing access-to-information requests, the trail went cold.
The Regina Qu’Appelle Health Authority would only provide statistics, telling W5 that there were nine reported incidents of staff-to-resident abuse in 2013 for the entire health authority.
No dates, names of homes or other details of those incidents were provided.
When it comes to disclosing information about incidents of staff-to-resident abuse and neglect in nursing homes, Saskatchewan lags far behind provinces, such as Ontario, where all incident reports are available online.
Some details like personal information are redacted but one can easily determine what is happening inside care homes. Only Quebec was worse, providing no information whatsoever.
Saskatchewan accounted for 30 of the nearly 1,500 staff-on-resident abuse incidents W5 was able to compile from our access requests to health authorities and provinces across the country.

“Certainly we would have the ability to look at what other provinces do when it comes to being more transparent, and disclosing more information to the public,” Saskatchewan Health Minister Dustin Duncan told W5, when asked about his province’s secrecy.
Province or Territory Reported Incidents
- Newfoundland and Labrador 3
- Prince Edward Island 0
- New Brunswick 10
- Nova Scotia 36
- Ontario 1,111
- Manitoba 59
- Saskatchewan 30
- Alberta 113
- British Columbia 138
- Northwest Territories 1
- Nunavut 1
- Yukon 0
- Total 1,502
Under-reporting of incidents
When W5 shared its findings with experts in seniors’ care we were told that actual numbers are likely higher due to under-reporting.
Lynn McDonald of the University of Toronto’s Institute for Life Course and Aging told Sandie Rinaldo: “There is a management issue of secrecy. There’s no encouragement for anybody to report anything or do anything because they’ll just get in trouble as these people know.”

Seeking more information, W5 conducted an anonymous, national on-line survey of care workers in nursing homes over a period of four months.
We asked three main questions:
- In the past year, have you witnessed staff-to-resident abuse (verbal, physical, emotional, sexual, financial) in the nursing home where you work?
- To whom did you first report the incident?
- Is the staff member who you witnessed abusing a resident still employed at the nursing home where you work?
We received 677 responses, with most coming from Ontario which seemed to confirm the experts’ opinions that many incidents go un-reported:
- 38% reported having witnessed one of their colleagues abusing a resident
- Only 51% said they reported abuse they had witnessed to a manager or administrator
- More than 80% said that the staff member they had seen abusing a resident was still employed at the facility
In Regina, Margaret Warholm’s family were not satisfied by the responses they received from Santa Maria, the care home where she died.
They took their concerns to the Saskatchewan legislature, holding a news conference to complain that a lack of care was a factor in her death.

Soon, their complaints had ballooned into a political crisis for the government and Duncan was forced to ask the provincial ombudsman to initiate an investigation into care homes.
The investigation was later expanded to include all long-term care across Saskatchewan. It is still underway but to date the Ombudsman has received 79 complaints.
Watch W5 Saturday @ 7 p.m. or online at CTVNews.ca/W5 after the televised airing.
Documents obtained by W5 will be posted Saturday @ 7 p.m.
Litsa Sourtzis and Steve Bandera , W5 Staff
Published Friday, April 10, 2015 3:30PM EDT
I just caught this issue of W5 for the first time today and am absolutely appalled. I worked with the elderly (in a community setting, not a medical or residential facility – 1985-1994) and nothing in these videos qualifies as excusable behaviour by any set of criteria. They are simply, tragically, assaults. I don’t buy the argument that no intent could be determined from the perpetrators’ actions. What I saw in this program was a lack of political will to move forward with criminal prosecution.The standards of behaviour in any field are specific to that field, and the care of the elderly and/or infirm includes consciously modifying caregiver behaviour to take care-recipients’ specific physical and emotional/mental needs into account. To willfully ignore or dismiss those standards when the result is injury or death is evidence of intent. To willfully countermand medically ordered treatment (e.g., that a bedridden patient not be transferred) endangering a patient’s well being is evidence of intent. To lie about the extent of injury resulting from a perpetrator’s actions is evidence of intent. While it is a trusim to state that only the guilty hide their actions, we are well beyond the point where lobbying for transparency and accountability will have a noticeable effect on care in time to prevent future unnecessary suffering and tragedy. We need a country-wide elder-abuse lobby to bring politicians to account about their own negligence in regulating this industry. I am now a professional writer and editor living in Calgary, Alberta. If anyone on the W5 team who worked on this program know of an agency/organization or group that could use my services in furtherance of this goal, I officially give you permission to forward my email address to them, so they may contact me.